On the heels of my criticism of Seligman’s portrayal of psychology as the science of mental disease, it seems appropriate to address the question What is a Mental Disorder? This is a hot issue right now because the Diagnostic and Statistical Manual of Mental Disorders is in the process of making a major revision, from IV-R to V. In that regard, authors are considering some significant changes to the definition of mental disorder. The definition is a crucial issue for mental health professionals and society in general for many different reasons, including who has access to care and how we think about the nature of the human condition. Given the complex nature of the issues and the fragmentation and conceptual confusion in psychology (and, yes, psychiatry), it should not come as a surprise that there is much confusion and controversy regarding what exactly constitutes a mental disorder. (See, for example, this article by Gary Greenberg).
Here are some basic questions regarding the definition of a mental disorder:
Where is the line between normal variation and pathology? Are mental disorders categorically different or are do they simply exist at the extremes of a continuum?
Does having a mental disorder say anything about one’s character or should it be completely separated from that, and thus the individual should not be judged or stigmatized? What if the disorder is a personality disorder? Doesn’t that, by definition, say the structure of a person’s character is a problem?
Are mental disorders natural kinds that can be objectively specified or are they entirely the result of social values and the cultural construction of what is normal (i.e., different values will lead to different conceptions of what is a mental disorder)?
Are mental disorders essentially like other disease or illnesses in medicine or are they a fundamentally different kind of condition?
This last question is particularly important from the vantage point of psychiatry relative to other mental health professions. Psychiatrists are, of course, medical doctors, and there is thus much pressure for psychiatry to perceive mental disorders as akin to other medical conditions. Yet many mental health professionals, like professional psychologists, counselors, social workers, and marriage and family therapists are neither trained in medicine nor inclined to want to reduce the problems they see to dysfunctional biology.
If you wonder whether this issue has real consequences, check out an open letter about the upcoming DSM revisions from the Division of Humanistic Psychology. The essence of the letter is the concern about medicalizing human problems and suffering and framing the nature of mental disorders in a biologically reductionistic way. (By the way, I signed the petition).
One of my earliest articles (here in word form finalHD) grounded in the unified theory was on the question of what is a mental disorder and focused especially on the issue of whether mental disorders were of the same essential kind as other biological diseases. My answer was that some mental disorders are likely reducible to (neuro) biological dysfunction that produces harmful consequences. Consider, for example, a rather obvious case like Alzheimer’s disease. Other highly likely candidates for what I call mental diseases are autism, schizophrenia, severe cases of OCD, Bipolar 1.
On the flip side, there are many mental disorders that cannot be reduced to or understood in terms of biological malfunction. Instead, these conditions are maladaptive psychological behaviors (often of a cyclical nature) that result in excessive (or clinically significant) levels of distress and dysfunction for the individual and/or society. (The value of the article for me was affirmed when I received a call out of the blue from Bob Spitzer, primary author of the DSM III and IV and told me he thought the analysis was convincing).
I have explored the nature of disorder in some depth via the construct of depression. In an article arguing that we should consider depression a state of behavioral shutdown, I pointed out how different portrayals result in radically different notions of what the term depression means.
“To get a flavor for why depression might mean different things to different researchers and how those different meanings might carry different sociopolitical implications, imagine two different television commercials. The first begins with an attractive woman isolating herself at a party. Everyone else appears to be having a good time, yet she stands in the background, ostensibly gripped in the throes of a seemingly inexplicable sadness. The cultural milieu is of upper middle class suburbia. A soft voice inquires and informs, “Have you experienced periods of depressed mood? Have you lost interest in things you used to enjoy? Do you feel tired, guilty, ineffective or hopeless? Depression is an illness. Ask your doctor about new antidepressant treatments available.” The implicit message of this commercial is clear. When people are suffering from depression, something has gone wrong with the physiology of the brain.
“Now imagine a different commercial. This one begins with an impoverished woman getting slapped by her husband. Her three children are having difficulties in school. Her husband controls her, and she has little in the way of social support. She recently immigrated to the United States and cannot get a job because she only speaks a little English. She frequently faces prejudice and racism. The voice overlay asks, “Have you been feeling down or depressed, guilty or hopeless? Have you lost interest in things you usually enjoy? Depression is an illness. Ask your doctor about new antidepressant treatments available.” Somehow the “depression as disease” message in this commercial is less convincing.”
I teach my doctoral students that depression is a state of behavioral shutdown. That behavioral shutdown needs to be placed in the developmental historical context to determine its nature. I further argue that, given the nature and context of the shutdown, we can further consider whether depression should be thought of as a normal reaction (in the case of extreme loss, humiliation, or chronic traumatization), part of a vicious psychological cycle (some stress or loss results in maladaptive shutting down which results in further problems and the failure to effectively adapt to the environment) or depressive diseases (when the shutdown is pervasive and occurs independent of context or changes in the environment).
This is a complicated construct with many possible threads and implications and I welcome thoughts, questions, or additional issues to be considered.
Gregg
Comments on: "What is a Mental Disorder?" (9)
I think the more interesting implication of the first commercial is that not being the life of the party is a medical problem. Why wouldn’t our first instinct be that the person at the periphery is normal, and all the people in the center are manic, or at a clinical extreme on the extroversion scale?
Now that I’ve outed myself….
I agree with everything you say, but I’m not sure this puts psychology in a place that is much different from medicine. That is, I think psychology suffers from a bad understanding of how medicine works, at least as much as it suffers from the medical model being inappropriate. Lets say you are a doctor, and someone comes into your office and presents with near deadly levels of some chemical in their blood stream (salt, cholesterol, or something more exotic). Sometimes the correct response is to give them medicine that helps their body process such chemicals more effectively, or blocks it from being absorbed. Other times the correct response is to address their environment, perhaps by altering their diet. Still other times the correct response is address a seemingly unrelated issue (perhaps a brain tumor pressing their pituitary gland, or simply getting them to drink more water throughout the day). And of course, still other times, we tell the person that given unalterable aspects of their circumstances all seems fairly normal. Even if it is not normal, we might tell them that the downsides of treatment don’t really make sense given their circumstances.
Back to psychology: If we agree that depressed woman number one has no reason to be depressed, we might just give her a few pills. If we agree that depressed woman number two probably should be depressed, given her circumstances, we can focus our intervention on the circumstances, or at least on her relationship with the circumstances. I’m not saying either of those treatments would be the right thing to do, I’m just saying it doesn’t seem very different from what a good medical doctor does.
Hi Eric,
Interesting comment about the commercials and it made me chuckle and reflect. In a separate article on the relationship between psychology and politics (written by myself and Steve Quackenbush), we make the offhand comment that depression might be caused by a lucid awareness of the human condition…:o). Although not directly parallel, your comment reminded me of that.
I also agree with what I take to be your point about medical doctors. It is easy to idealize the precision with which they operate, and it is also the case that they do many different kinds of interventions, many of which parallel what professional psychologists (or other health care professions do). I note this every time I visit my own physician.
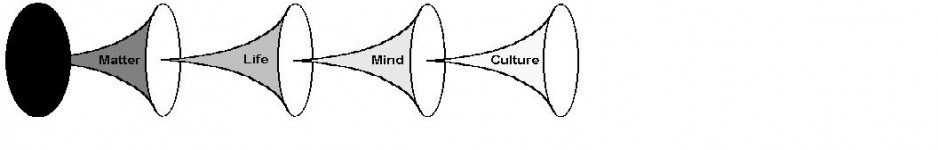
My point, which I am guessing you would agree with, is that medicine should be thought of as studying, analyzing, and altering the biological dimension of human complexity. Of course, to do so requires knowledge and analysis of psychological and social dimensions, but the primary focus and training of medical doctors is on the biological dimension. In parallel, professional psychologists need to understand the biological and social dimensions of psychological functioning (the behavior of the individual as a whole), but nevertheless they focus on the psychological level.
Gregg
There’s another basic question that could be asked about the concept of “mental disorder”, as well:
Is the concept of “mental disorder” even a valid concept in the first place?
If not, then that might help explain why “…there is much confusion and controversy regarding what exactly constitutes a mental disorder”.
Hi Jason,
It is an interesting question and I think all psychiatrists and professional psychologists should be familiar with Thomas Szasz, the most famous skeptic of the construct. Are you thinking here of his argument that mental illness is a myth that is not grounded in sound models of function and dysfunction (he argued that real biological disorders have lesions) but instead represented a form of social control of deviants? The third question touches on this, but I hear you suggesting we back further up, and start with whether the whole construct is justifiable. As I wrote in the article differentiating mental disorder from disease, I agree that it is not a pure natural science construct, but I do believe it is a necessary utilitarian construct. If you disagree with that, I would be interested in hearing the argument…
Peace,
Gregg
Hi Gregg,
Well, first I think the concepts of “mental disorder/disease/illness” are just blatant category errors. The implication of such terminology is that the concepts, “biological” and “mental” are in the same category — an implication that I find so obviously and patently absurd that I can’t see how anyone takes it seriously in the first place.
Secondly, there’s the issue of the meaning of the constituent concepts of “mental disorder”. As an analogy, if someone says “red car”, then the implication is that one knows the meaning Of both “red” and “car”. If one does not know the meaning of even one of those words, (either “red” or “car”), then that someone certainly isn’t going to know the meaning of the two words put together. By the same token, you could get a dozen psychologists together, ask them the meaning of “mental” and “disorder”, and most likely get a dozen different answers for each word, and therefore those same psychologists are certainly in no position to talk about “mental disorder”.
Thirdly, the implication of the concept, “mental disorder”, (along with the erroneous notion that it is a *scientific* concept), is that it is a concept that it is ultimately grounded in *fact* when it is indeed a concept that is ultimately grounded in *value*. Every so-called “mental disorder” is implicitly referring to a set of behaviors that not only “ought not be”, but also behaviors that “ought not be” that also need professional *intervention* of some sort or another.
To put it bluntly, the “mental disorder” concept is implicitly and ultimately reflective of a particular *value system* that merely poses as a scientific construct. (Indeed, it is a pseudoscientific concept.) And this is where its “utilitarian” aspects come into play. For to say that something has “utility” is to say that that something is “useful”. But to say that something is “useful” is to further imply that that something is *useful to some end*. And whenever we speak of “ends”, we are speaking of a state of affairs that currently *is not* but *ought to be*, which is ultimately a question of *value*.
Thus, the psychology/psychiatric community needs to make their implicit value system *explicit* and **JUSTIFY** that value system, (i.e., what are “the ends” of the psychological and psychiatric community?). After *justifying* that value system, they then need to make explicit those behaviors that “ought not be to the point of needing professional intervention”, and *justify* that, as well. After justifying that position, they then need to decide the appropriate *means to those ends*, and explicitly justify that.
In the end, the only utility that the “mental disorder” concept has is to relieve the psychological/psychiatric community of *the responsibility* to explicity justify a value system that is implicit in that concept. The medicalization of certain behaviors is precisely the means by which to do that, for it gives that value system the mere appearance of being scientific, (and therefore the appearance of being grounded in *fact*), when it categorically is no such thing.
—Jason B.
Hi Jason,
I have mixed reactions to your comments here. I agree with several key elements, but I think it is too generally dismissive of the concept. Your post seems to imply there is no such thing as mental illness/disease/disorder. The brain is a complicated system, it breaksdown, we observe breakdowns at the level of mental behavior. For example, I have an elderly member of my extended family right now who is experiencing massive decline in her mental functioning, demonstrating problems in memory, hallucinations, paranoia, aggressive outbursts. I would say she is mentally ill. Her mental system is breaking down. And, as a clinician who often works with people with severe mental illness, this is not a terribly unusual phenomena. So, I think the concept of mental illness/disorder/disease is a necessary one.
I would take that argument a step further. There are people who are miserable, suffering, and adjusting to the stressors and affordances in their lives in a maladaptive way. They can not will themselves out of their suffering, and treatment from a professional is a valid notion, one that is, speaking generally empirically documented to help (evidence is clear that psychotherapy reduces suffering).
I agree with the following:
1. There is not good consenual agreement, I believe this is in large part because of the massive conceptual confusion in psychology.
2. The has been a ‘bio’ medicalization of many mental disorders in a way that has been inappropriate. I say ‘bio’ because for many people, medical is akin to health, and many of them use a biopsychosocial model of illness. For example, talk to nurses about their conception of health. Bottom line is that there are broad and narrow definitions of the term medical, which leads to confusion. Many mental disorders are not biomedical conditions.
3. In lines with #2, there are many mental health problems that are not reducible to biological dysfunction, and that many people make category errors in describing psychological problems as biological disease-like entities.
4. Many people are suffering at the psychological (individual/small group, behavioral investment & justification) level of analysis, therapy helps, and we need the institution of mental health.
5. The DSM is generally lame for the purposes of doing psychology on what I call the neurotic problems (these are problems of identity, relationship and affect–depression and anxiety), and I applauded the development of the Psychodynamic Diagnostic Model, at least in theory. I hope one day that we will have a diagnostic model for psychological problems.
6. As you note, the concept of mental disorder must be a utilitarian construct. This is a hugely key point and everything you say is on target about the need for our profession to EXPLICITLY justify our value system and what we believe people ought to be like. My motto for living, BE THAT WHICH ENHANCES DIGNITY AND WELL BEING WITH INTEGRITY speaks to this issue for me. Psychology has done some work on this, but not nearly enough. I think our doc program at JMU does a good job heightening students awareness of this issue.
I am curious to get your thoughts…
G
Hi Gregg,
You wrote: “Your post seems to imply there is no such thing as mental illness/disease/disorder.”
JasonB: Not exactly. What I’m basically saying is that I don’t think that *the terminology* of mental illness/disease/disorder is the appropriate terminology for what that terminology is intended to refer to.
Gregg: “The brain is a complicated system, it breaksdown, we observe breakdowns at the level of mental behavior.”
JasonB: I would frame it a little differently. I would say something like, “The brain is a complicated system, it breaksdown, and we *infer the possibility* of brain ‘breakdowns’ at the observed level of mental behavior.”
In regards to the unfortunate state of affairs of your elderly extended family member, I would agree that her “mental system is breaking down”. I would also say that it is (most certainly) her *brain/nervous system* that is “breaking down”, and that this is the cause of her mental system breaking down, (i.e., the mental system breakdown is an effect). Thus, and insofar that the problem has a **biological** cause, it seems more appropriate to say something like *neuronal* illness/disorder/disease, for these terms imply a *biological* breakdown. Basically, this is a semantic issue for me.
Gregg: I would take that argument a step further. There are people who are miserable, suffering, and adjusting to the stressors and affordances in their lives in a maladaptive way.
Jason: I completely agree. But this does not necessarily mean that utilizing terms like illness/disorder/disease necessarily follow from such a state affairs. Interestingly, a term like “maladaptive” would probably be more on the right track…
Gregg: They can not will themselves out of their suffering, and treatment from a professional is a valid notion, one that is, speaking generally empirically documented to help (evidence is clear that psychotherapy reduces suffering).
Jason: Again, I do not disagree. My concern is about labelling people in such a state of affairs as “ill” or “disordered” or “diseased” only because they are suffering to such a degree that they cannot will themselves out of it.
Gregg,
Jason beat me to it, but I think you are missing the point to his criticism. Attempting a slightly different tact…
Let’s assume that we all agree that some people have problems properly described as “psychological” – they feel undue suffering, have trouble doing things they seem capable of doing, experience things is highly abnormal ways, etc.
Now, the issue is whether it is helpful to consider those issues using the metaphor that they are like medical diseases. Maybe a mechanical model would be better: When a car engine has a trouble charging the battery, we don’t say that it suffers from “alternator deficiency syndrome.” We say that the alternator is “broken” and “needs repairs.” Maybe a more systems level model would be better: When animals in a river are dieing because of too much fertilizer run off, we don’t say that it has a “failure to thrive disorder”. Instead we talk about the organisms being “unable to properly adapt to a new equilibrium”, or might even talk about a “chemical imbalance”. There are many other options available, or we could make our own.
The question is: What, if anything, do we gain by thinking that psychological problems are analogous to medical problems, and in what ways can it be misleading.
Well… the concept is definitely valid when taken more literally. That is, some people’s minds are not as ordered as others. People with some types of schizophrenia, for example, have particularly dis-ordered minds.
The term becomes a bit more awkward when it becomes more metaphorical. For example, if someone declared that a person with sever OCD has a disorder, you might well reply “all evidence to the contrary, his mind seems terrifically ordered.”
Of course, even under the more literal usage, we might still wonder about whether or not we should be in the mind-ordering business. But such again, we are in the same boat as medicine. It is no more or less obvious that we should be in the blood filtering business, or the kidney transplanting business.